Introduction to Vasoconstriction and Thermoregulation
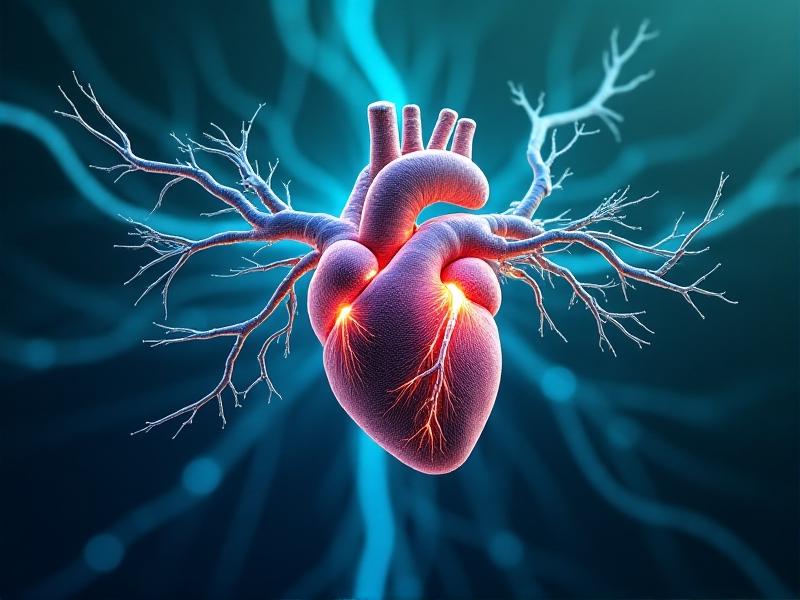
When exposed to cold, the human body activates a cascade of physiological responses to preserve core temperature. Central to this process is vasoconstriction—the narrowing of blood vessels—which reduces blood flow to the skin and extremities, minimizing heat loss. This adaptive mechanism is a cornerstone of thermoregulation, ensuring vital organs remain functional even in frigid conditions. Understanding how vasoconstriction operates under cold stress reveals the delicate balance between survival and vulnerability in extreme environments.
The Physiological Mechanism Behind Cold-Induced Vasoconstriction
Vasoconstriction is orchestrated by the sympathetic nervous system, which releases norepinephrine to bind to alpha-adrenergic receptors on smooth muscle cells lining blood vessels. This triggers contraction, reducing vessel diameter and redirecting blood toward the core. Simultaneously, cold-sensing transient receptor potential (TRP) channels in the skin send signals to the hypothalamus, the body's thermostat, to coordinate systemic responses. Hormones like adrenaline further amplify this reaction, ensuring rapid adaptation to temperature drops.
How the Body Detects and Responds to Cold
Specialized thermoreceptors in the skin detect temperature changes and relay information via sensory nerves to the brainstem and hypothalamus. The hypothalamus integrates these signals and initiates autonomic responses, including shivering and vasoconstriction. This feedback loop ensures real-time adjustments: as core temperature stabilizes, vasoconstrictive intensity may moderate, but prolonged cold exposure keeps these defenses active. Remarkably, this system prioritizes survival over comfort, often sacrificing peripheral tissues to safeguard the heart, brain, and lungs.
Regional Variations in Vasoconstrictive Responses
Not all body regions constrict blood vessels equally. Fingers, toes, ears, and the nose experience pronounced vasoconstriction due to their high surface-area-to-volume ratio, which accelerates heat loss. In contrast, the torso and head receive preferential blood flow. This spatial hierarchy explains why frostbite typically affects extremities first. Additionally, repeated cold exposure can induce adaptive heterogeneity—individuals like ice swimmers often develop enhanced peripheral tolerance through training.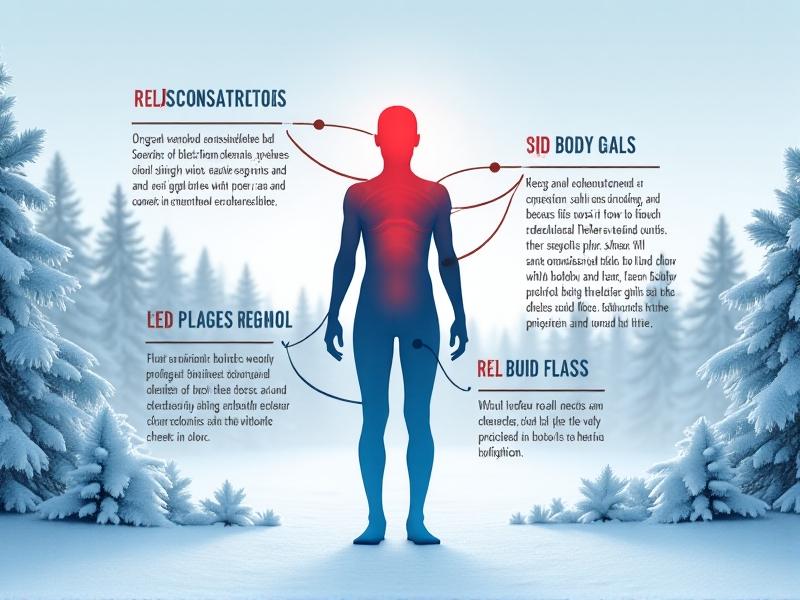
Health Implications: Benefits and Risks
Controlled vasoconstriction during brief cold exposure can boost metabolic rate, improve circulation resilience, and enhance stress adaptation. Athletes use ice baths to reduce inflammation and accelerate recovery. However, chronic vasoconstriction poses risks: elevated blood pressure, reduced nutrient delivery to tissues, and heightened cardiovascular strain. Individuals with Raynaud’s syndrome or hypertension may experience exacerbated symptoms, underscoring the need for balanced cold exposure practices.Vasoconstriction in Hypothermia and Frostbite
In hypothermia, vasoconstriction becomes maladaptive as prolonged reduction in peripheral blood flow lowers core temperature further, creating a vicious cycle. Frostbite occurs when ice crystals form in tissues deprived of warmth and oxygen, causing cellular damage. Early stages involve painful vasoconstriction; numbness follows as nerves deteriorate. Immediate rewarming is critical, but refreezing must be avoided to prevent irreversible injury.Acute vs. Chronic Cold Exposure Adaptations
Acute cold exposure triggers immediate but transient vasoconstriction, whereas chronic exposure induces long-term adaptations. Populations in polar regions exhibit enhanced vasoconstrictive efficiency and increased brown fat activation, which generates heat non-shiveringly. Athletes and cold-workers also develop tolerance through acclimatization, demonstrating the body’s remarkable plasticity. However, these adaptations require gradual exposure to avoid overwhelming physiological systems.Practical Applications: Sports, Medicine, and Survival
Vasoconstriction principles inform practices from cryotherapy to wilderness survival. Mountain climbers use mittens to counter peripheral vasoconstriction, while surgeons employ localized cooling to reduce bleeding. Emerging research explores cold exposure for treating inflammatory disorders. Understanding these dynamics equips individuals to harness cold’s benefits while mitigating risks—whether optimizing performance or enduring extreme conditions.Advertisement
Recommended Reading: Cold Water Exposure for Jet Lag Recovery



















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *