The Science Behind Post-Cold Therapy Rewarming
Post-cold therapy, such as cryotherapy or ice baths, relies on controlled exposure to extreme cold to reduce inflammation, numb pain, and stimulate recovery. However, the rewarming phase is equally critical. Rapid or improper rewarming can lead to tissue damage, thermal shock, or diminished benefits. The body’s natural response to cold involves vasoconstriction—narrowing blood vessels to conserve heat. Rewarming reverses this process, gradually restoring circulation and preventing stress on the cardiovascular system. Understanding this balance ensures safety and maximizes therapeutic outcomes.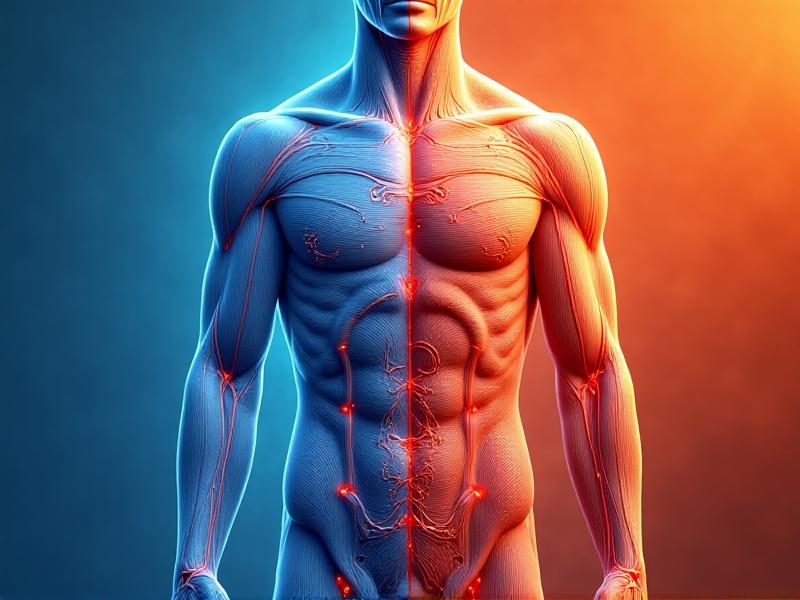
Passive Rewarming: Letting the Body Recover Naturally
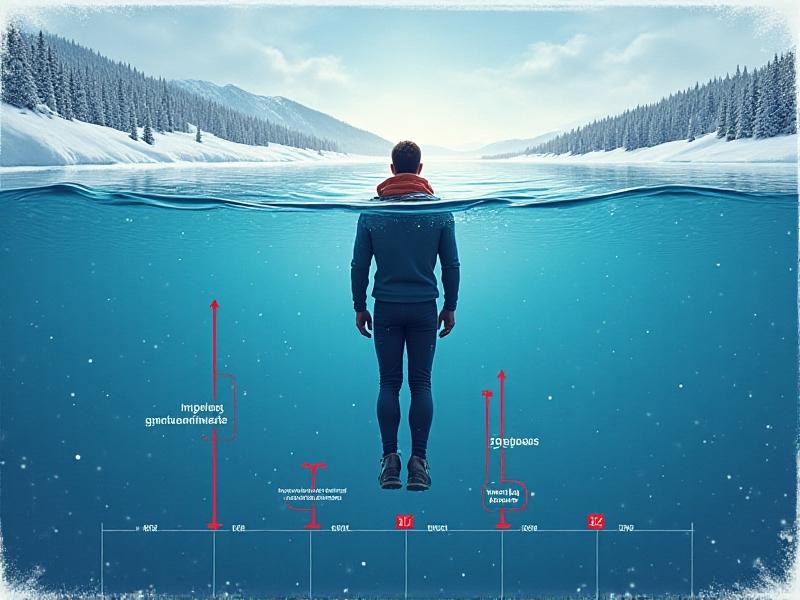
Passive rewarming relies on the body’s inherent ability to generate heat through metabolic processes. This method involves moving to a warm environment, wearing dry clothing, and resting. Ideal for mild cold exposure, it minimizes risks like abrupt temperature changes. Studies show passive rewarming maintains stable blood pressure compared to aggressive techniques. However, it’s slower—taking 30–60 minutes—and less effective for severe hypothermia. Best paired with light movement or calorie intake to boost heat production.
Active External Rewarming: Blankets, Heat Packs, and Warm Baths
Active external methods apply direct heat to the skin’s surface. Electric blankets, heated pads, or warm water immersion (38–42°C) accelerate recovery by widening blood vessels. Hydrotherapy baths are popular among athletes for reducing muscle stiffness post-cryotherapy. However, excessive heat can cause burns or rebound inflammation. A 2022 meta-analysis recommends limiting sessions to 15–20 minutes and monitoring skin response. For localized cold injuries, targeted heat packs work best without overwhelming the body.
Active Internal Rewarming: Advanced Medical Interventions
Reserved for extreme cases, active internal methods use medical tools like warmed intravenous fluids or airway heating devices. These bypass the skin to deliver heat directly to the core, raising body temperature by 1–2°C per hour. Hospitals often pair them with external techniques for synergistic effects. While highly effective for hypothermia, their invasiveness and cost make them impractical for routine post-cold therapy. DIY approaches, like drinking warm fluids, offer a safer, accessible alternative.
Contrast Therapy: Balancing Cold and Heat
Contrast therapy alternates between cold and warm stimuli—for example, switching from an ice bath to a sauna. This “pumping” effect enhances circulation, flushing metabolic waste while reducing swelling. A 2021 study found 3–4 cycles of 2 minutes cold/3 minutes heat optimal for muscle recovery. However, individuals with cardiovascular issues should avoid rapid shifts. Infrared saunas provide a gentler alternative, using radiant heat to promote gradual vasodilation without extreme temperature swings.Hydration and Nutrition: Fueling Recovery from Within
Rewarming increases metabolic demand, making hydration and nutrient intake essential. Warm beverages like herbal tea or broth boost core temperature while replenishing fluids. Carbohydrates and proteins provide energy for thermogenesis; oatmeal or lentil soup are ideal post-therapy meals. Electrolyte-rich drinks combat dehydration from sweating during active rewarming. Avoid alcohol—it impairs circulation and delays recovery.The Role of Gentle Movement and Massage
Light exercises like yoga or walking reactivate muscles without strain, promoting even heat distribution. Massage therapy enhances this by manually stimulating blood flow—a 2023 trial showed 20 minutes of kneading improved rewarming speed by 25%. Foam rollers and percussion devices offer DIY alternatives. Focus on major muscle groups, using circular motions to avoid bruising.Common Mistakes to Avoid During Rewarming
Rapid rewarming—like using a hairdryer or hot shower—can cause capillary damage and numbness. Overheating in saunas risks fainting; always monitor time and temperature. Ignoring shivering (a natural heat-generator) delays recovery. Dressing too tightly restricts circulation. Instead, prioritize gradual warmth and listen to physiological cues.Evaluating Effectiveness: Which Method Comes Out on Top?
For most, passive rewarming paired with hydration offers a safe baseline. Athletes benefit from contrast therapy’s efficiency, while medical scenarios demand active internal methods. Cost, accessibility, and individual health dictate the best approach. Combining techniques—like a warm bath followed by light stretching—often yields optimal results without undue risk.Advertisement
Recommended Reading: Portable Cold Plunge Solutions for Travel


















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *