Understanding Pediatric Cold Exposure Risks
 Children are more vulnerable to cold exposure than adults due to their smaller body mass and higher surface-area-to-volume ratio, which accelerates heat loss. Infants and toddlers, in particular, lack the ability to regulate body temperature efficiently, making them prone to hypothermia even in mildly cold conditions. Risks vary by age, activity level, and environmental factors like wind chill. Understanding these risks is critical; studies show that cold-related pediatric ER visits spike during winter months, often due to inadequate preparation or prolonged outdoor play.
Children are more vulnerable to cold exposure than adults due to their smaller body mass and higher surface-area-to-volume ratio, which accelerates heat loss. Infants and toddlers, in particular, lack the ability to regulate body temperature efficiently, making them prone to hypothermia even in mildly cold conditions. Risks vary by age, activity level, and environmental factors like wind chill. Understanding these risks is critical; studies show that cold-related pediatric ER visits spike during winter months, often due to inadequate preparation or prolonged outdoor play.
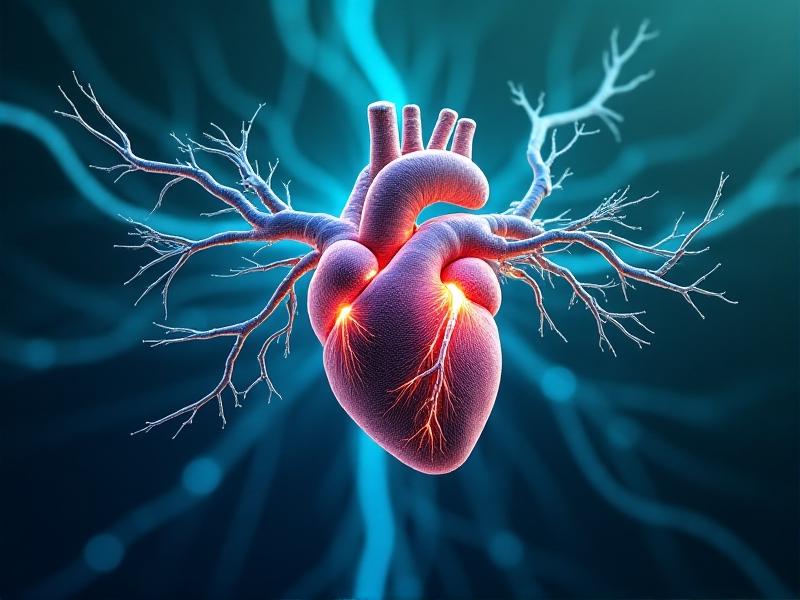
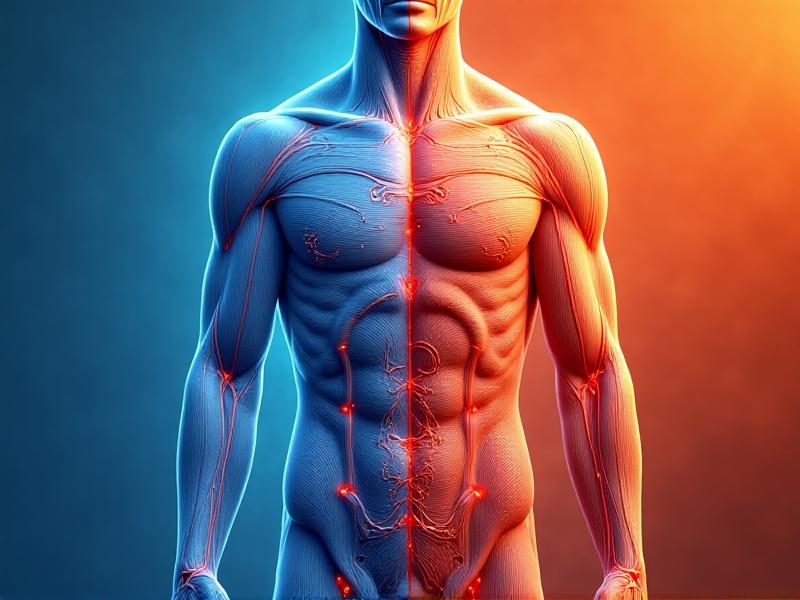
Physiology of Children in Cold Environments
 Children’s bodies respond differently to cold. Their faster metabolic rates generate heat quickly but also expend energy rapidly, leaving them susceptible to exhaustion. Infants rely on brown adipose tissue for thermogenesis, but this diminishes with age. Blood vessels in extremities constrict sooner in cold to preserve core warmth, increasing frostbite risk. Thin subcutaneous fat layers offer minimal insulation, and their inability to articulate discomfort often delays intervention. Recognizing these physiological nuances helps caregivers implement proactive protective measures.
Children’s bodies respond differently to cold. Their faster metabolic rates generate heat quickly but also expend energy rapidly, leaving them susceptible to exhaustion. Infants rely on brown adipose tissue for thermogenesis, but this diminishes with age. Blood vessels in extremities constrict sooner in cold to preserve core warmth, increasing frostbite risk. Thin subcutaneous fat layers offer minimal insulation, and their inability to articulate discomfort often delays intervention. Recognizing these physiological nuances helps caregivers implement proactive protective measures.
Age-Specific Guidelines for Cold Exposure
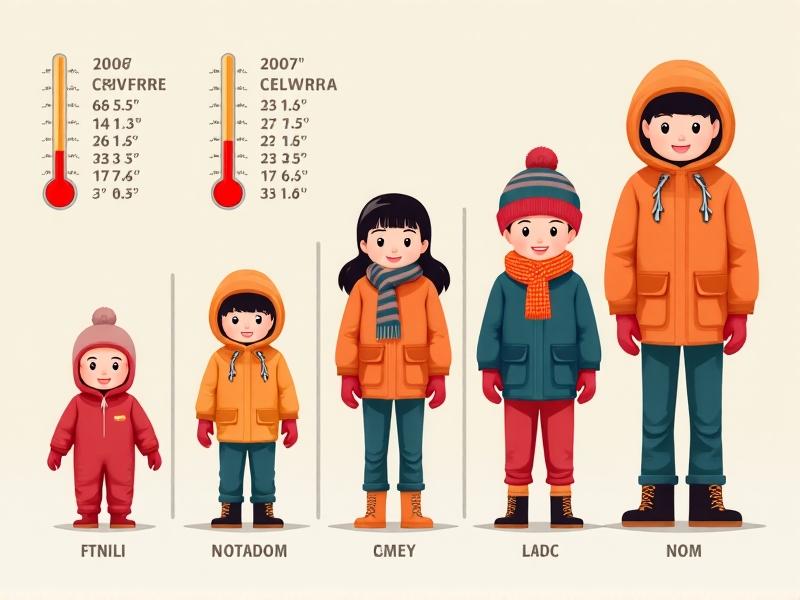 Infants under 12 months should avoid outdoor exposure in temperatures below freezing. If necessary, limit outings to 10–15 minutes with layers, insulated carriers, and covered skin. Toddlers (1–3 years) require frequent indoor breaks every 20–30 minutes. School-aged children can handle longer durations but need dry clothing and hydration. Adolescents may overexert themselves in sports; enforce rest periods and moisture-wicking fabrics. The American Academy of Pediatrics advises canceling outdoor activities if wind chill drops below -27°F (-32°C), as frostbite can occur within 30 minutes.
Infants under 12 months should avoid outdoor exposure in temperatures below freezing. If necessary, limit outings to 10–15 minutes with layers, insulated carriers, and covered skin. Toddlers (1–3 years) require frequent indoor breaks every 20–30 minutes. School-aged children can handle longer durations but need dry clothing and hydration. Adolescents may overexert themselves in sports; enforce rest periods and moisture-wicking fabrics. The American Academy of Pediatrics advises canceling outdoor activities if wind chill drops below -27°F (-32°C), as frostbite can occur within 30 minutes.
Recognizing Hypothermia and Frostbite Symptoms
 Hypothermia in children begins with shivering, slurred speech, and clumsiness. Severe cases involve slowed breathing, weak pulse, and lethargy. Frostbite appears as numbness, redness, or grayish-yellow skin on fingers, toes, ears, or nose. Infants may exhibit unusual quietness or refusal to feed. Immediate action includes moving indoors, replacing wet clothing, and gradual warming using blankets or skin-to-skin contact. Avoid direct heat sources like hot water, which can burn sensitive skin. Persistent symptoms warrant urgent medical care.
Hypothermia in children begins with shivering, slurred speech, and clumsiness. Severe cases involve slowed breathing, weak pulse, and lethargy. Frostbite appears as numbness, redness, or grayish-yellow skin on fingers, toes, ears, or nose. Infants may exhibit unusual quietness or refusal to feed. Immediate action includes moving indoors, replacing wet clothing, and gradual warming using blankets or skin-to-skin contact. Avoid direct heat sources like hot water, which can burn sensitive skin. Persistent symptoms warrant urgent medical care.
Layering and Clothing Strategies for Winter
Effective layering combines a moisture-wicking base (e.g., polyester or wool), an insulating middle layer (fleece or down), and a windproof outer shell. Avoid cotton, which traps moisture. Mittens trump gloves for warmth retention; pair with waterproof boots and thermal socks. Cover 90% of skin in extreme cold—balaclavas protect faces, while neck gaiters prevent heat loss. For infants, use one additional layer than an adult would wear. Overheating risks sweating, so check for damp collars or backs and adjust layers accordingly.Safe Outdoor Activities in Cold Weather
Prioritize short, engaging activities like sledding or snowman-building. Avoid static play (e.g., waiting in lines) to maintain circulation. Set time limits based on temperature: 20-minute intervals at 20°F (-6°C), shorter if windy. Supervise adolescents skiing or skating to prevent overexertion. Hydrate frequently—cold air dehydrates faster than perceived. Teach older kids to recognize numbness or fatigue as signals to head indoors. Always have a warm vehicle or shelter nearby for emergencies.Indoor Safety and Recovery Post-Cold Exposure
Post-outdoor recovery starts with gradual rewarming. Offer lukewarm drinks like broth or cocoa to raise core temperature. Remove damp clothing immediately; use dry blankets or a pre-warmed bath (not exceeding 104°F/40°C). Monitor for “afterdrop”—a dangerous post-rewarming temperature plunge caused by cold blood returning to the core. Apply moisturizer to wind-chapped skin, and watch for persistent shivering or confusion. Encourage rest to replenish energy stores depleted by cold stress.Common Myths About Cold Weather and Children
Myth: “Cold air causes illness.” Truth: Viruses spread more in indoor crowds, not cold itself. Myth: “More layers equal more warmth.” Overbundling restricts movement and traps sweat. Myth: “Rub frostbitten skin.” Rubbing damages tissues; instead, soak in warm water. Myth: “Alcohol warms you up.” It dilates blood vessels, increasing heat loss. Dispelling these myths ensures caregivers prioritize evidence-based strategies over folklore, improving winter safety outcomes.Emergency Response and When to Seek Help
Call 911 if a child shows severe hypothermia (unconsciousness, shallow breathing) or deep frostbite (blisters, blackened skin). While waiting, insulate them from the ground, avoid jarring movements, and provide CPR if needed. For mild frostbite, immerse affected areas in warm (not hot) water until sensation returns. Document symptoms’ onset and duration for medical staff. Post-rescue, schedule a follow-up with a pediatrician to address potential complications like nerve damage or infection.Advertisement
Recommended Reading: Blood Pressure Monitoring During Ice Baths




















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *