The Critical Role of Immune Cell Proliferation in Modern Medicine
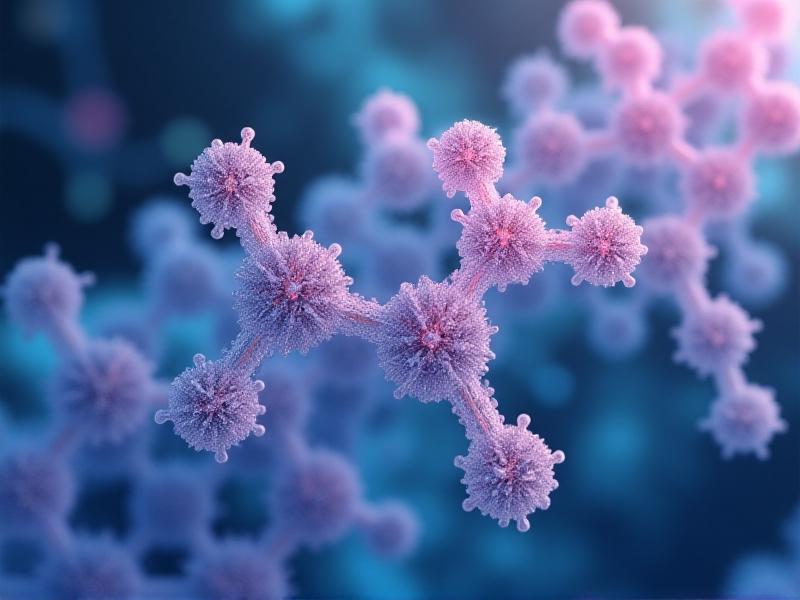
Immune cell proliferation lies at the heart of the body’s defense mechanisms, orchestrating responses to infections, cancers, and autoimmune disorders. Clinical studies in this field explore how immune cells like T-cells, B-cells, and natural killer (NK) cells multiply and differentiate, offering insights into therapies for diseases once deemed untreatable. From cancer immunotherapies to vaccines, understanding these processes has revolutionized medical science. This article delves into the science, methodologies, and transformative potential of immune cell proliferation research.
Molecular Mechanisms Driving Immune Cell Expansion
Immune cell proliferation is governed by complex molecular pathways. Cytokines like interleukins (IL-2, IL-7) and growth factors activate signaling cascades, such as the JAK-STAT pathway, which regulate cell division and differentiation. Checkpoint proteins like PD-1 and CTLA-4 act as brakes, preventing excessive immune responses. Dysregulation of these mechanisms can lead to autoimmune diseases or immunodeficiency. Recent studies highlight the role of metabolic reprogramming—how immune cells shift their energy production to meet proliferation demands—a breakthrough for enhancing CAR-T cell therapies.
Methodologies in Clinical Immune Cell Research
Cutting-edge tools like flow cytometry and single-cell RNA sequencing enable researchers to track proliferating immune cells with unprecedented precision. Imaging techniques such as multiphoton microscopy visualize real-time cell interactions in living tissues. In vivo models, including humanized mice, provide platforms to test therapies like checkpoint inhibitors. Clinical trials now leverage biomarkers like Ki-67 to quantify proliferation rates, correlating them with patient outcomes. These methodologies are pivotal in optimizing treatments such as allogeneic stem cell transplants.
Therapeutic Applications: From Cancer to Autoimmunity
Cancer immunotherapies like CAR-T cells rely on engineered T-cell proliferation to eradicate tumors. Drugs like nivolumab (anti-PD-1) unleash suppressed immune cells, while therapies for autoimmune diseases aim to curb pathological proliferation. For example, JAK inhibitors mitigate rheumatoid arthritis by blocking pro-inflammatory signals. Emerging approaches include ex vivo expansion of tumor-infiltrating lymphocytes (TILs) for reinfusion, showing promise in metastatic melanoma. These advances underscore the duality of immune proliferation—balancing activation and restraint is key.
Challenges in Clinical Translation
Despite progress, challenges persist. Overactive immune proliferation can trigger cytokine release syndrome (CRS), a life-threatening complication of CAR-T therapy. Heterogeneity in patient responses—due to genetic variability or tumor microenvironment differences—complicates treatment standardization. Long-term durability of responses remains another hurdle; some patients relapse as tumors evolve escape mechanisms. Researchers are exploring combination therapies and predictive algorithms to address these issues, aiming for personalized regimens.Future Directions: Precision and Innovation
The future lies in precision medicine. CRISPR-Cas9 gene editing could enhance immune cell specificity, reducing off-target effects. AI-driven platforms analyze vast datasets to predict proliferation patterns and optimize drug combinations. Trials exploring in vivo CAR-T generation—where vectors engineer a patient’s own cells without ex vivo steps—are underway. Additionally, microbiome research reveals how gut bacteria influence immune cell dynamics, opening new therapeutic avenues. These innovations aim to make immune cell therapies safer, more effective, and widely accessible.Final Thoughts
Immune cell proliferation research is reshaping modern medicine, offering hope where traditional therapies fall short. By unraveling molecular intricacies and leveraging novel technologies, clinicians are turning once-fatal diseases into manageable conditions. Yet, the journey from bench to bedside demands careful navigation of biological complexities. As science advances, the synergy between innovation and clinical rigor will continue to unlock the full potential of the immune system—a testament to the power of cellular life.Advertisement
Recommended Reading: Cold Therapy vs Cryotherapy Chamber Efficacy




















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *