The Hypothalamus: Master Regulator of Homeostasis
 Nestled deep within the brain, the hypothalamus acts as a biological command center, weighing barely four grams yet governing critical processes like temperature regulation, hunger, thirst, and sleep cycles. This almond-sized structure bridges the nervous and endocrine systems, translating neural signals into hormonal directives. Its ability to adapt to repeated stressors—whether psychological, metabolic, or environmental—forms the cornerstone of survival. By constantly monitoring internal states through specialized neurons, the hypothalamus fine-tunes bodily responses, demonstrating a remarkable plasticity that challenges earlier notions of static neural pathways.
Consider how morning light exposure gradually trains the hypothalamus to anticipate wakefulness. Over days and weeks, the suprachiasmatic nucleus—the body’s master clock—adjusts melatonin production, illustrating how persistent stimuli reshape hypothalamic function. This adaptability extends to metabolic processes, where recurrent overeating dampens leptin sensitivity, altering how the brain perceives satiety. Such changes aren’t glitches but evolutionary safeguards, allowing organisms to thrive under varying conditions.
Modern research reveals that these adaptations occur through epigenetic modifications and synaptic remodeling. Repeated exposure to specific triggers activates gene networks that either reinforce or dampen particular pathways. For instance, chronic stress reprograms corticotropin-releasing hormone neurons, permanently altering stress response thresholds. This biological balancing act underscores why understanding hypothalamic plasticity matters—it holds keys to addressing obesity, PTSD, and circadian disorders.
Nestled deep within the brain, the hypothalamus acts as a biological command center, weighing barely four grams yet governing critical processes like temperature regulation, hunger, thirst, and sleep cycles. This almond-sized structure bridges the nervous and endocrine systems, translating neural signals into hormonal directives. Its ability to adapt to repeated stressors—whether psychological, metabolic, or environmental—forms the cornerstone of survival. By constantly monitoring internal states through specialized neurons, the hypothalamus fine-tunes bodily responses, demonstrating a remarkable plasticity that challenges earlier notions of static neural pathways.
Consider how morning light exposure gradually trains the hypothalamus to anticipate wakefulness. Over days and weeks, the suprachiasmatic nucleus—the body’s master clock—adjusts melatonin production, illustrating how persistent stimuli reshape hypothalamic function. This adaptability extends to metabolic processes, where recurrent overeating dampens leptin sensitivity, altering how the brain perceives satiety. Such changes aren’t glitches but evolutionary safeguards, allowing organisms to thrive under varying conditions.
Modern research reveals that these adaptations occur through epigenetic modifications and synaptic remodeling. Repeated exposure to specific triggers activates gene networks that either reinforce or dampen particular pathways. For instance, chronic stress reprograms corticotropin-releasing hormone neurons, permanently altering stress response thresholds. This biological balancing act underscores why understanding hypothalamic plasticity matters—it holds keys to addressing obesity, PTSD, and circadian disorders.
Neuroplasticity in the Hypothalamic Circuitry
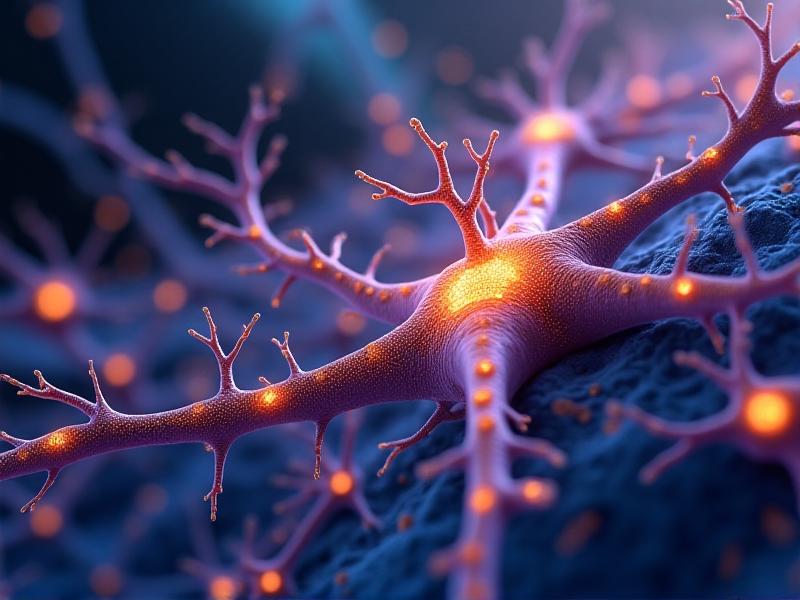 Unlike rigid computer circuits, the hypothalamus thrives on change. Its neurons rewire connections in response to repeated stimuli through mechanisms like long-term potentiation and dendritic arborization. Stress studies in rodents demonstrate how chronic corticosterone exposure shrinks hippocampal neurons while expanding dendritic trees in the amygdala—a pattern mirrored in hypothalamic stress-response circuits. These structural shifts enable the brain to prioritize survival-oriented behaviors, albeit sometimes at the cost of long-term health.
Orexin-producing neurons exemplify this plasticity. Typically regulating wakefulness and appetite, these cells adjust their firing patterns under sleep deprivation. After successive nights of disrupted sleep, their activity blunts, reducing alertness signals—a maladaptive response contributing to chronic fatigue. Similarly, repeated exposure to high-fat diets dulls POMC neuron responsiveness to insulin, creating a vicious cycle of overeating and metabolic dysfunction.
Advanced imaging techniques now capture these changes in real time. Optogenetics reveals how specific hypothalamic nuclei recruit auxiliary neurons when faced with persistent challenges. This redundancy explains why some adaptations become entrenched while others remain reversible. Pharmaceutical interventions targeting these plasticity mechanisms—like mTOR inhibitors—are showing promise in resetting maladaptive pathways in preclinical trials.
Unlike rigid computer circuits, the hypothalamus thrives on change. Its neurons rewire connections in response to repeated stimuli through mechanisms like long-term potentiation and dendritic arborization. Stress studies in rodents demonstrate how chronic corticosterone exposure shrinks hippocampal neurons while expanding dendritic trees in the amygdala—a pattern mirrored in hypothalamic stress-response circuits. These structural shifts enable the brain to prioritize survival-oriented behaviors, albeit sometimes at the cost of long-term health.
Orexin-producing neurons exemplify this plasticity. Typically regulating wakefulness and appetite, these cells adjust their firing patterns under sleep deprivation. After successive nights of disrupted sleep, their activity blunts, reducing alertness signals—a maladaptive response contributing to chronic fatigue. Similarly, repeated exposure to high-fat diets dulls POMC neuron responsiveness to insulin, creating a vicious cycle of overeating and metabolic dysfunction.
Advanced imaging techniques now capture these changes in real time. Optogenetics reveals how specific hypothalamic nuclei recruit auxiliary neurons when faced with persistent challenges. This redundancy explains why some adaptations become entrenched while others remain reversible. Pharmaceutical interventions targeting these plasticity mechanisms—like mTOR inhibitors—are showing promise in resetting maladaptive pathways in preclinical trials.
Stress Adaptation and the HPA Axis Rewiring
 The hypothalamus-pituitary-adrenal axis operates like a biological alarm system, fine-tuned through evolution to handle acute threats. But modern life’s unrelenting pressures—from work deadlines to social media overload—test this ancient machinery. Initial stress spikes cortisol, sharpening focus and energy mobilization. However, repeated activation flattens the cortisol curve, leaving individuals in a zombified state of chronic fatigue and emotional numbness.
Animal studies reveal startling neuronal changes after sustained stress. Vasopressin-producing cells in the paraventricular nucleus hypertrophy, flooding the system with stress hormones even after threats subside. Meanwhile, glucocorticoid receptors in the hippocampus atrophy, impairing negative feedback loops. This dual dysfunction creates a self-perpetuating stress cycle that’s evident in conditions like treatment-resistant depression.
Emerging therapies aim to reboot HPA axis regulation. Fasting protocols and cold exposure therapies—though seemingly counterintuitive—appear to rebuild stress resilience by imposing controlled challenges. Early adopters report improved cortisol rhythms, suggesting these practices might counteract hypothalamic burnout. Pharmaceutical approaches focus on modulating CRH receptors, with several novel antagonists entering phase III trials for anxiety disorders.
The hypothalamus-pituitary-adrenal axis operates like a biological alarm system, fine-tuned through evolution to handle acute threats. But modern life’s unrelenting pressures—from work deadlines to social media overload—test this ancient machinery. Initial stress spikes cortisol, sharpening focus and energy mobilization. However, repeated activation flattens the cortisol curve, leaving individuals in a zombified state of chronic fatigue and emotional numbness.
Animal studies reveal startling neuronal changes after sustained stress. Vasopressin-producing cells in the paraventricular nucleus hypertrophy, flooding the system with stress hormones even after threats subside. Meanwhile, glucocorticoid receptors in the hippocampus atrophy, impairing negative feedback loops. This dual dysfunction creates a self-perpetuating stress cycle that’s evident in conditions like treatment-resistant depression.
Emerging therapies aim to reboot HPA axis regulation. Fasting protocols and cold exposure therapies—though seemingly counterintuitive—appear to rebuild stress resilience by imposing controlled challenges. Early adopters report improved cortisol rhythms, suggesting these practices might counteract hypothalamic burnout. Pharmaceutical approaches focus on modulating CRH receptors, with several novel antagonists entering phase III trials for anxiety disorders.
Metabolic Memory: When the Hypothalamus Can't Forget
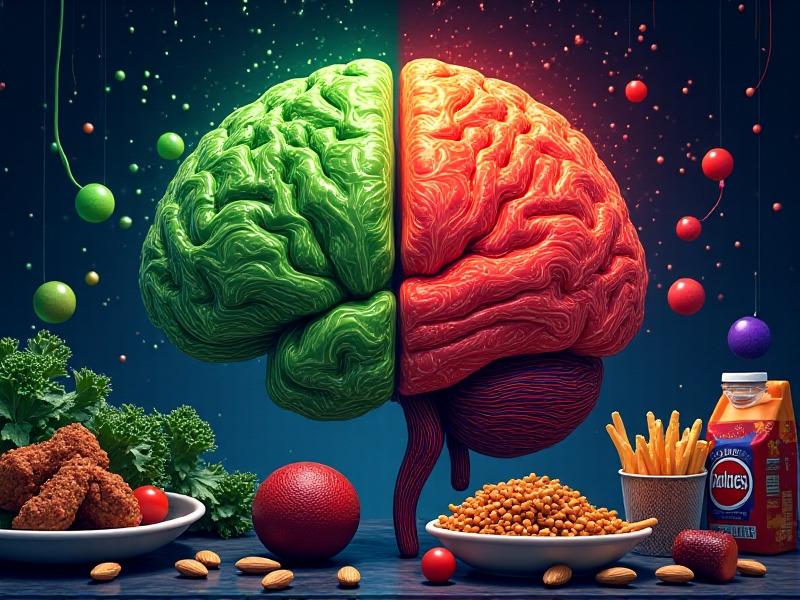 The hypothalamus maintains energy balance through a delicate dance between hunger hormones. Ghrelin surges trigger foraging behavior, while leptin signals fat storage adequacy. But repeated exposure to hyperpalatable foods hijacks this system—high-fructose diets reduce hypothalamic leptin receptors by 40% within weeks in primate studies. This mimics the pathophysiology seen in human obesity, where the brain becomes “blind” to satiety signals.
Time-restricted eating experiments reveal the hypothalamus’s capacity to reset. Mice on high-fat diets but confined to 8-hour feeding windows maintain leptin sensitivity compared to unrestricted peers. Human trials show similar promise—participants report normalized hunger cues within weeks of structured meal timing. These findings suggest metabolic plasticity persists despite prior damage, offering hope for lifestyle interventions.
Drug development now targets hypothalamic nutrient sensing. GLP-1 agonists like semaglutide don’t just slow gastric emptying; they cross the blood-brain barrier to directly enhance POMC neuron activity. Combined with dietary approaches, these medications might reverse decades of metabolic adaptation, though long-term effects require further study.
The hypothalamus maintains energy balance through a delicate dance between hunger hormones. Ghrelin surges trigger foraging behavior, while leptin signals fat storage adequacy. But repeated exposure to hyperpalatable foods hijacks this system—high-fructose diets reduce hypothalamic leptin receptors by 40% within weeks in primate studies. This mimics the pathophysiology seen in human obesity, where the brain becomes “blind” to satiety signals.
Time-restricted eating experiments reveal the hypothalamus’s capacity to reset. Mice on high-fat diets but confined to 8-hour feeding windows maintain leptin sensitivity compared to unrestricted peers. Human trials show similar promise—participants report normalized hunger cues within weeks of structured meal timing. These findings suggest metabolic plasticity persists despite prior damage, offering hope for lifestyle interventions.
Drug development now targets hypothalamic nutrient sensing. GLP-1 agonists like semaglutide don’t just slow gastric emptying; they cross the blood-brain barrier to directly enhance POMC neuron activity. Combined with dietary approaches, these medications might reverse decades of metabolic adaptation, though long-term effects require further study.
Circadian Entrainment: Beyond Light and Dark Cycles
Shift workers and frequent flyers experience firsthand the hypothalamus’s struggle to adapt to conflicting Zeitgebers. While light remains the primary circadian cue, emerging research highlights secondary influences—consistent meal times strengthen peripheral clock genes, while social interactions modulate suprachiasmatic nucleus output. This layered entrainment explains why some individuals weather time zone changes better than others. Chronic circadian disruption triggers insidious changes. Mouse studies show that six months of shifted light cycles cause irreversible dendritic loss in orexin neurons, paralleling human narcolepsy pathology. Similarly, rotating shift workers exhibit shrunken hypothalamic volumes on MRI—a possible contributor to their elevated dementia risk. These findings underscore the need for circadian hygiene in an always-on society. Circadian-focused therapies are gaining traction. Timed melatonin supplementation (not just dosage) improves shift worker alertness by 60% in clinical trials. More radically, controlled light exposure protocols are helping neurodegenerative patients regain daily rhythms, suggesting intact hypothalamic plasticity even in advanced disease states.Harnessing Hypothalamic Plasticity in Clinical Practice
Understanding hypothalamic adaptation is revolutionizing obesity treatment. Researchers now view regained weight not as personal failure but biological inevitability—the hypothalamus actively defends elevated set points through altered energy expenditure and hunger signaling. Bariatric surgery’s lasting success appears rooted in resetting these set points, possibly via altered gut-brain axis signaling that overrides existing adaptations. In mental health, trauma-focused therapies are incorporating hypothalamic resilience training. Biofeedback devices measuring skin conductance and heart rate variability help patients recognize stress adaptation patterns, allowing intentional reprocessing of traumatic memories. Early PTSD trials combining these methods with neurofeedback show a 50% greater remission rate compared to traditional exposure therapy. Neurological rehabilitation also benefits from this paradigm. Stroke protocols now include hypothalamic stimulation to enhance neuroplasticity, leveraging its role in growth factor regulation. Preliminary results indicate a 30% acceleration in motor recovery when paired with physical therapy, suggesting widespread therapeutic potential.Frontiers in Hypothalamic Adaptation Research
The next decade promises unprecedented insights into hypothalamic function. Single-cell RNA sequencing has already identified 62 hypothalamic neuron subtypes previously lumped together. This granular understanding allows targeted interventions—researchers recently reversed age-related metabolic decline in mice by rejuvenating a specific POMC neuron cluster using genetic tools. Nanotechnology introduces new modulation possibilities. Injectable “neurostaples” that mechanically stimulate hypothalamic regions are being tested for obesity, bypassing pharmacological side effects. Early animal data shows a 20% weight reduction sustained six months post-treatment, though human trials remain years away. Ethical questions loom as manipulation deepens. Should we enhance hypothalamic function in healthy individuals to optimize performance? As optogenetic wearables enter consumer markets, society must grapple with the neuroethics of democratized brain adaptation—a frontier as challenging as the science itself.Advertisement
Recommended Reading: Water Displacement Calculations for Plunge Tubs
























Comments
Leave a Comment
Your email address will not be published. Required fields are marked *