Understanding Cold Urticaria: The Science Behind the Reaction
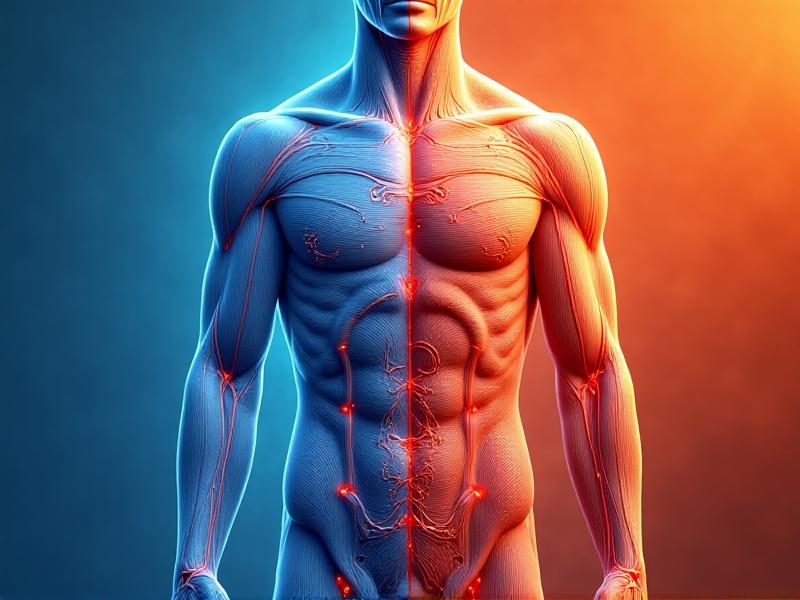
Cold urticaria is a rare condition where exposure to cold temperatures triggers an allergic response, resulting in hives, swelling, or even anaphylaxis. This occurs when mast cells in the skin release histamine in reaction to cold stimuli, such as cold air, water, or surfaces. The exact cause remains unclear, but researchers believe genetic factors, underlying autoimmune conditions, or viral infections may play a role. Understanding this pathophysiology is crucial for developing effective management strategies, especially during immersion in cold environments like swimming or winter sports.
Identifying Triggers: Environmental and Activity-Specific Risks
Triggers vary widely among individuals. Immersion in cold water, even briefly, can provoke severe reactions. Activities like ice bathing, surfing, or walking in chilly rain heighten risks. Ambient factors such as wind chill or rapid temperature shifts (e.g., moving from a warm room to cold air) also exacerbate symptoms. Recognizing personal thresholds through controlled exposure tests under medical supervision helps tailor prevention plans. Journaling incidents, including duration and environmental conditions, can pinpoint patterns and refine risk avoidance.
Pre-Immersion Preparation: Layering and Barrier Techniques
Layering clothing creates insulation while allowing flexibility. Start with moisture-wicking base layers, add thermal mid-layers, and finish with windproof, water-resistant outerwear. For water-based activities, neoprene wetsuits or drysuits provide critical thermal barriers. Covering extremities with gloves, waterproof boots, and balaclavas minimizes skin exposure. Applying petroleum-based ointments to exposed areas like the face can add a protective layer. Always carry emergency thermal blankets and warming packs to counteract sudden temperature drops during immersion.
Medication and Emergency Protocols: Antihistamines and Beyond
Non-sedating antihistamines like cetirizine or loratadine are frontline treatments to reduce histamine release. For severe cases, doctors may prescribe leukotriene inhibitors or omalizumab. Carrying an epinephrine auto-injector is essential for anaphylaxis risk. Before immersion, discuss a personalized action plan with an allergist, including pre-medication timing and post-exposure steps. Training companions to recognize symptoms—such as wheezing, dizziness, or swelling—ensures rapid response during emergencies.Gradual Acclimatization: Building Tolerance Safely
Controlled exposure under medical guidance may help desensitize the body. This involves brief, incremental cold contact—like holding an ice cube for 30 seconds—while monitoring reactions. Over weeks, duration and intensity can increase if tolerated. However, this approach isn’t universally effective and requires strict supervision. Pairing acclimatization with antihistamines or pre-warming techniques (e.g., light exercise) might enhance safety. Abandon the process if symptoms worsen or systemic reactions occur.
Post-Immersion Care: Warming Techniques and Symptom Monitoring
After cold exposure, rewarm the body gradually to avoid rapid vasodilation, which can worsen hives. Use warm (not hot) compresses and avoid direct heat sources like fireplaces. Hydrate with warm fluids and monitor for delayed reactions, such as joint pain or fatigue, which may indicate systemic involvement. Document symptoms for 24 hours to assess severity and adjust future plans. Consult a healthcare provider if inflammation persists or new symptoms arise.Psychological Strategies: Managing Anxiety Around Cold Exposure
Fear of reactions can lead to hypervigilance or avoidance of outdoor activities. Cognitive-behavioral therapy (CBT) techniques help reframe catastrophic thinking. Mindfulness practices, like grounding exercises during immersion, reduce panic. Support groups or counseling provide emotional validation and coping strategies. Balancing caution with confidence—through thorough preparation and contingency planning—fosters resilience and empowers individuals to engage in cold environments without excessive fear.Technology and Tools: Wearables for Real-Time Monitoring
Wearable devices like temperature-sensitive wristbands or smartwatches with environmental sensors alert users to unsafe conditions. Apps logging weather data, such as wind speed or humidity, help predict risks. Portable thermometers check water or surface temperatures before contact. Emerging research explores biosensors that detect early histamine surges, though these are not yet widely available. Combining tech with traditional methods creates a robust safety net.Case Studies: Learning from Real-Life Management Successes
A 28-year-old surfer with cold urticaria modified her routine by wearing a custom 7mm wetsuit and taking antihistamines 90 minutes before sessions. She avoids dawn patrols when temperatures plummet and uses a buddy system. Another case involves a hiker who acclimatized over six months to tolerate 10°C hikes without reactions. These examples underscore the importance of customization, patience, and integrating medical advice with practical adaptations.Future Directions: Research and Innovations in Treatment
Studies exploring monoclonal antibodies targeting IgE or interleukin-31 show promise in reducing hypersensitivity. CRISPR-based gene editing might one day address genetic contributors. Wearable biomimetic skins that regulate surface temperature autonomously are in early prototyping. Advocacy for greater awareness and funding is critical to accelerate these breakthroughs. Until then, combining existing strategies with vigilance remains the best approach for those navigating cold immersion.Advertisement
Recommended Reading: Cold Exposure Contraindications for Hypertensives



















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *