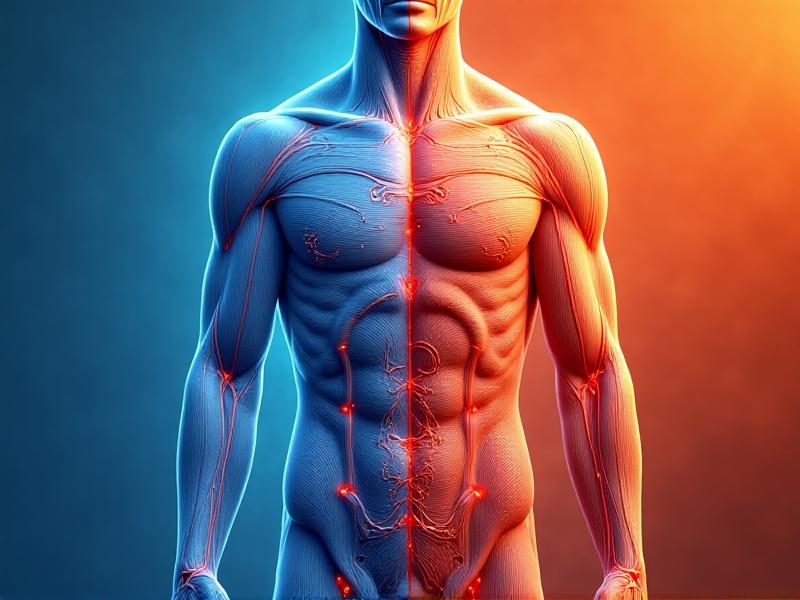
Understanding Autoimmune Conditions and Inflammation
Autoimmune conditions occur when the immune system mistakenly attacks the body’s own tissues, leading to chronic inflammation and tissue damage. Diseases like rheumatoid arthritis, lupus, and multiple sclerosis stem from this malfunction, often causing fatigue, pain, and mobility issues. Inflammation, a natural defense mechanism, becomes harmful when unregulated. Current treatments focus on suppressing immune activity, but emerging alternatives like cold exposure aim to modulate the immune response without complete suppression.
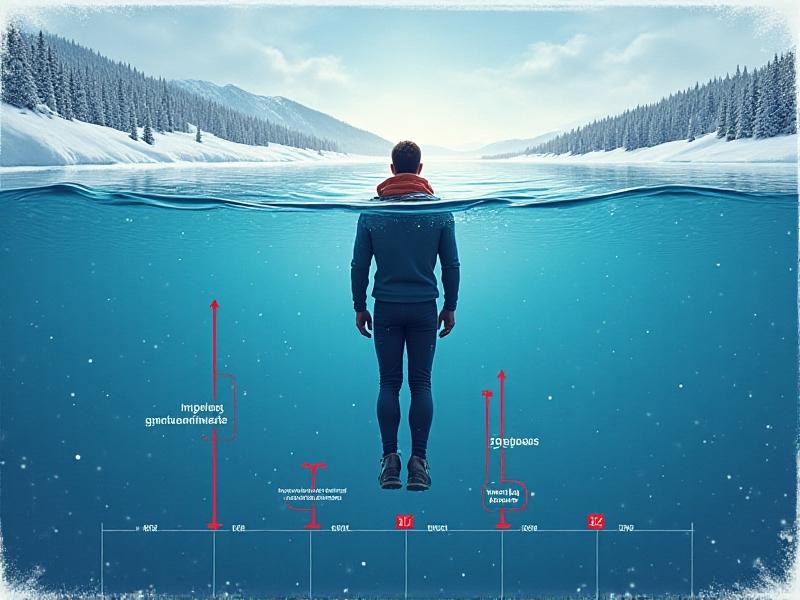
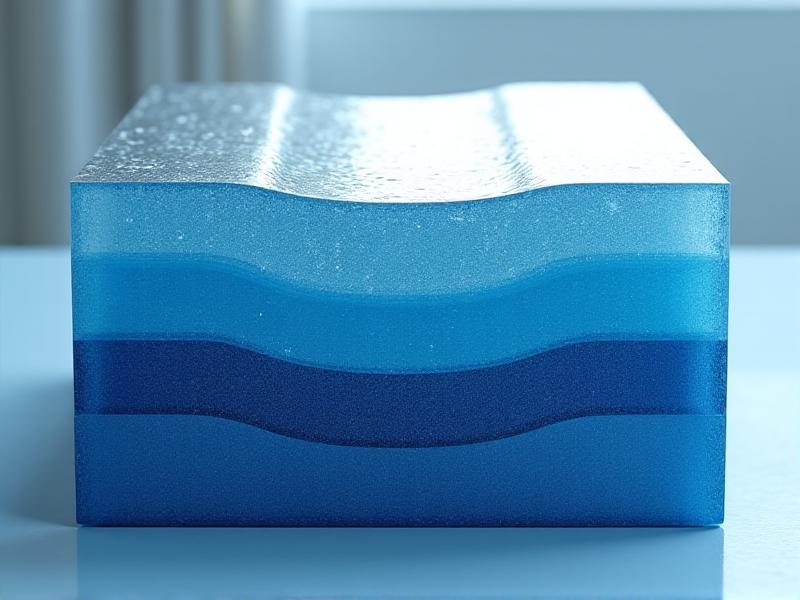
Introduction to Cold Exposure: Definitions and Methods
Cold exposure involves intentional immersion in cold environments or water to trigger physiological adaptations. Methods range from cold showers (50–60°F) to ice baths (40–50°F) and outdoor swims in natural bodies of water. Practices like the Wim Hof Method combine breathwork with cold therapy to enhance tolerance. These techniques stimulate the sympathetic nervous system, releasing norepinephrine and adrenaline, which may reduce inflammatory markers and improve stress resilience.
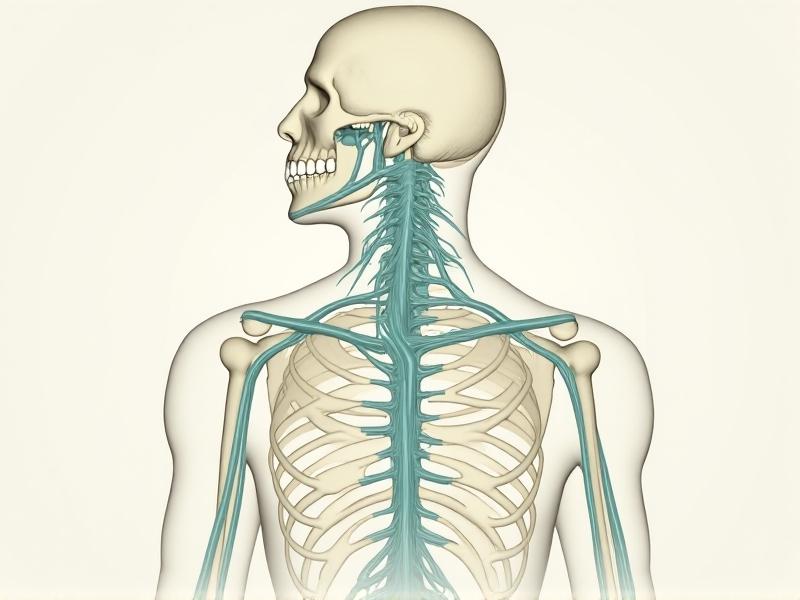
The Immune System’s Response to Cold
Cold exposure activates the body’s stress response, increasing production of anti-inflammatory cytokines like IL-10 while reducing pro-inflammatory ones like TNF-α. Studies suggest that repeated cold sessions can recalibrate immune activity, potentially preventing overactive responses in autoimmune patients. The vagus nerve, which modulates inflammation, may also be stimulated by cold, offering a pathway to balance immune function. This dual action—suppressing excessive inflammation while preserving defense mechanisms—makes cold therapy uniquely promising.
Cold Exposure Protocols for Autoimmune Management
Beginners should start with 30-second cold showers, gradually increasing to 2–5 minutes. Ice baths (10–15 minutes at 50°F) or outdoor immersion can follow. Consistency matters—3–4 sessions weekly—to sustain benefits. Pairing cold exposure with breathwork (e.g., slow diaphragmatic breathing) helps manage the stress response. Timing sessions in the morning may align with cortisol rhythms, enhancing anti-inflammatory effects. Always monitor symptoms and adjust duration based on personal tolerance.
Research Insights: Cold Therapy and Autoimmunity
A 2020 study found that cold-water immersion reduced IL-6 levels in athletes, suggesting anti-inflammatory potential. Another trial on rheumatoid arthritis patients noted decreased pain scores after 4 weeks of cold showers. While direct studies on autoimmune conditions are limited, anecdotal reports and mechanistic research highlight its plausibility. Researchers hypothesize that cold-induced norepinephrine may inhibit inflammatory pathways, offering a drug-free adjunct to traditional therapies.Comparing Cold Exposure with Other Therapies
Unlike immunosuppressants, cold therapy doesn’t broadly inhibit immunity but may recalibrate it. Compared to anti-inflammatory diets or stress-reduction practices, cold exposure offers a faster physiological stimulus. However, it’s less studied than established interventions. Combining cold therapy with meditation or yoga could synergistically reduce stress and inflammation, addressing multiple autoimmune triggers. It’s not a standalone cure but a complementary tool within a holistic plan.Safety Considerations and Contraindications
Cold exposure isn’t universally safe. Those with Raynaud’s phenomenon, cardiovascular issues, or severe hypothyroidism should avoid it. Gradual acclimatization prevents shock, and sessions should never exceed 15 minutes. Always consult a healthcare provider before starting, especially if using immunosuppressants. Signs to stop include numbness, dizziness, or prolonged shivering. Proper hydration and warm-up movements minimize risks.Patient Testimonials: Real-World Applications
Sarah, a lupus patient, reports fewer flare-ups after 6 months of daily cold showers. John, with rheumatoid arthritis, uses ice baths to reduce morning stiffness. These stories, while subjective, align with physiological research. Not everyone benefits—some find cold aggravates symptoms, underscoring the need for personalized approaches. Communities like autoimmune cold therapy groups provide support and shared strategies for experimentation.Building a Sustainable Cold Exposure Routine
Start slow: 10 seconds of cold water at shower’s end, increasing weekly. Track symptoms in a journal to gauge progress. Pair with mindfulness to enhance stress-buffering effects. Adapt methods to seasons—opt for outdoor swims in summer, shorter showers in winter. Consistency over intensity ensures long-term adherence. Celebrate small milestones, like completing a 1-minute ice bath, to stay motivated.Moving Forward: A Balanced Perspective on Cold Exposure
While promising, cold exposure isn’t a cure-all. Its role in autoimmune management lies in its potential to modulate inflammation and enhance resilience. Individual responses vary, requiring careful experimentation. Collaborating with healthcare providers ensures safety, while staying informed about emerging research helps refine practices. As interest grows, cold therapy may become a key player in integrative approaches to autoimmune health.Advertisement
Recommended Reading: Post-Cold Therapy Rewarming Methods Ranked




















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *