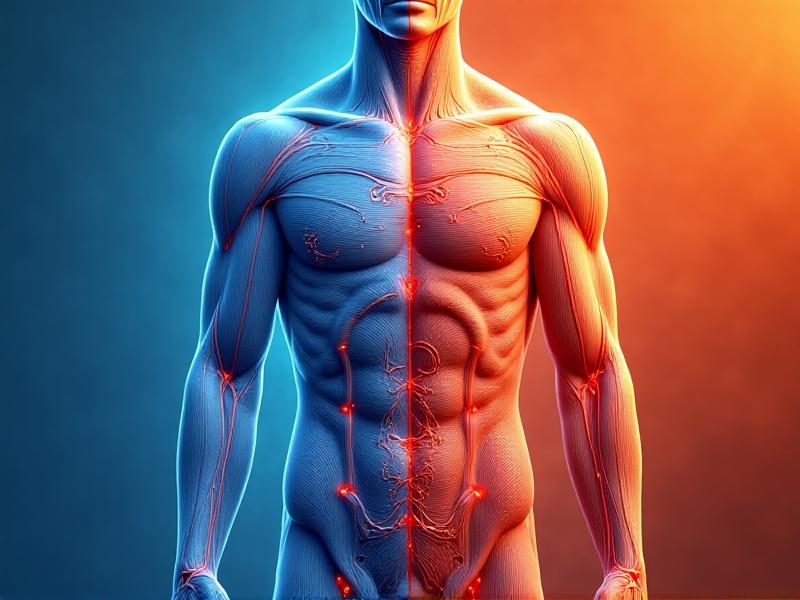
The Physiology of Cold Exposure and Blood Pressure
Cold exposure triggers a cascade of physiological responses designed to preserve core body temperature. One of the most immediate effects is vasoconstriction—the narrowing of blood vessels in the skin and extremities. This reduces heat loss but also increases peripheral resistance, forcing the heart to work harder to pump blood. Studies show that systolic blood pressure can rise by 10-20 mmHg within minutes of cold exposure, while diastolic pressure may increase by 5-15 mmHg. For individuals with hypertension, whose arteries already endure elevated pressure, this added strain can push their cardiovascular system into dangerous territory.
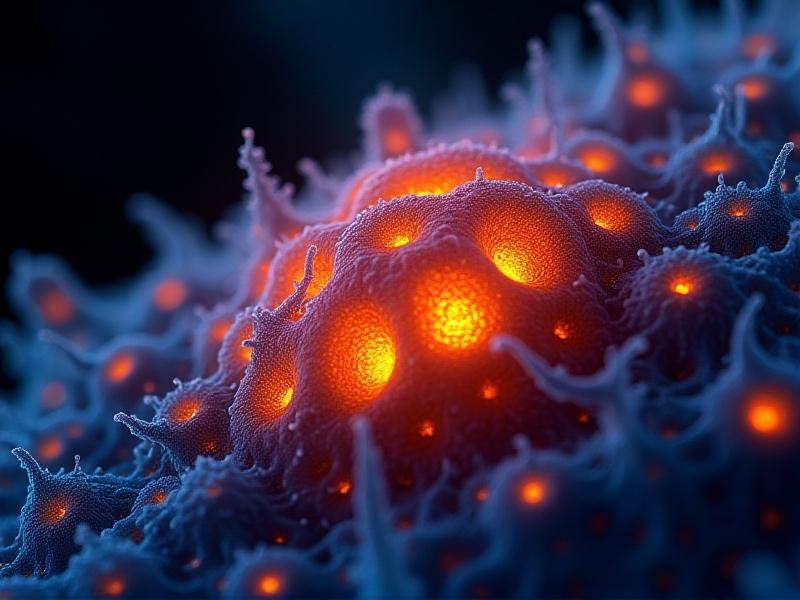
Why Hypertensives Are at Higher Risk
Hypertension damages arterial walls over time, reducing their elasticity and impairing the body’s ability to regulate blood pressure efficiently. When exposed to cold, the combined effects of vasoconstriction and adrenaline release create a "double burden" on the cardiovascular system. Research indicates that hypertensives experience sharper and more sustained blood pressure spikes compared to those with normal readings. These abrupt fluctuations heighten the risk of complications such as aortic dissection, stroke, or myocardial infarction, particularly in older adults or those with poorly controlled hypertension.
Potential Dangers of Cold Immersion and Activities
Cold-water immersion, winter sports, or even brisk walks in chilly weather can inadvertently become high-risk activities for hypertensives. Sudden immersion in cold water—popularized by wellness trends like ice baths—may trigger the mammalian dive reflex, slowing heart rate while simultaneously increasing blood pressure. This paradoxical response can destabilize cardiac rhythm in vulnerable individuals. Even routine activities like shoveling snow combine cold exposure with physical exertion, potentially spiking blood pressure beyond safe thresholds.
Guidelines for Saper Cold Exposure Practices
Hypertensives need not completely avoid cold exposure but should approach it with strategic precautions. Gradual acclimatization over weeks allows the body to adapt to colder temperatures without extreme spikes in blood pressure. Layering clothing to maintain consistent core temperature and covering extremities minimizes vasoconstriction. Monitoring blood pressure before and after exposure helps identify individual tolerance levels. Avoiding sudden temperature shifts—like stepping from a sauna into cold water—is critical, as these extremes amplify cardiovascular stress.
Alternative Therapies for Cardiovascular Health
For those seeking cold exposure’s purported benefits—like reduced inflammation or improved circulation—safer alternatives exist. Controlled heat therapy via saunas has been shown to lower blood pressure through vasodilation. Breathwork practices such as paced diaphragmatic breathing can enhance vascular function without temperature extremes. Moderate aerobic exercise in temperate environments also improves endothelial health, offering similar advantages to cold adaptation but with far lower cardiovascular risk.Case Studies: When Caution Prevails
A 58-year-old man with stage 2 hypertension ignored medical advice to discontinue ice baths, resulting in a hypertensive crisis that required emergency care. Conversely, a carefully monitored program for a 45-year-old woman with mild hypertension incorporated brief cool showers (20°C) after gradual acclimation, yielding improved stress response without blood pressure escalation. These examples underscore the importance of personalized approaches and professional guidance when navigating cold exposure with hypertension.Collaborating with Healthcare Providers
Open dialogue with clinicians helps hypertensives weigh risks against potential benefits. Providers may adjust antihypertensive medications seasonally, as some drugs like beta-blockers can impair thermoregulation. Regular ambulatory blood pressure monitoring during colder months provides data to tailor recommendations. Emerging technologies like wearable cardiovascular monitors now enable real-time tracking during cold exposure experiments, fostering evidence-based personal protocols.Advertisement
Recommended Reading: Alcohol Consumption Risks in Winter Swimming





















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *