The Rising Popularity of Ice Baths and Their Physiological Impact
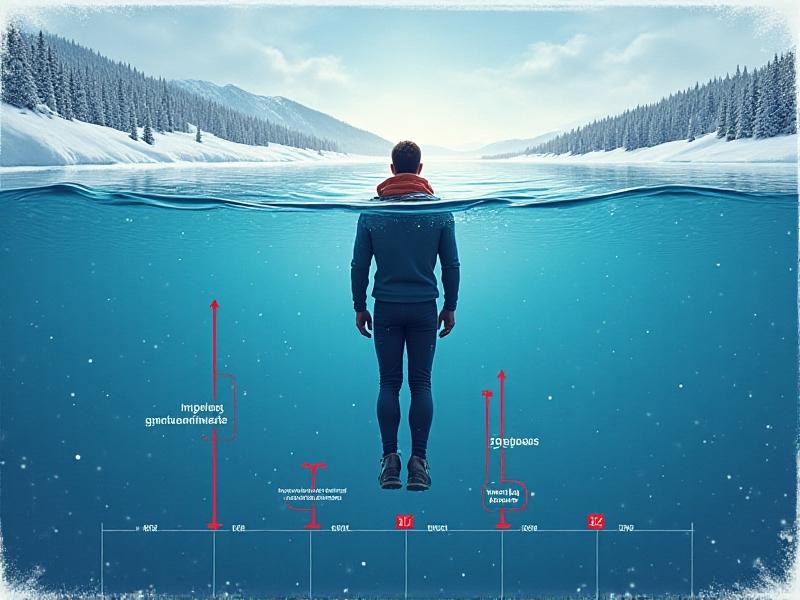
Ice baths, once reserved for elite athletes, have surged in popularity among fitness enthusiasts and wellness seekers. Immersing the body in cold water (typically 10–15°C) is believed to reduce muscle soreness, enhance recovery, and improve mental resilience. However, this practice isn’t without risks—especially concerning cardiovascular health. Sudden cold exposure triggers a cascade of physiological responses, including vasoconstriction and increased heart rate, which can lead to dramatic blood pressure fluctuations. Understanding these effects is critical for safely incorporating ice baths into recovery routines.
The Physiology of Cold Exposure and Blood Pressure
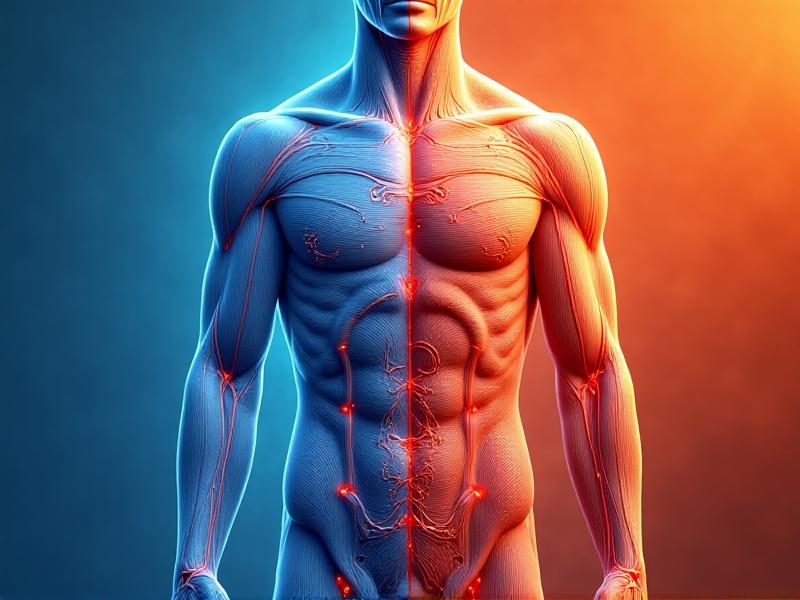
When the body encounters cold water, the sympathetic nervous system activates the “fight or flight” response. Blood vessels near the skin constrict to conserve heat, redirecting blood flow to vital organs. This vasoconstriction increases peripheral resistance, causing a temporary spike in blood pressure. Concurrently, the heart pumps harder to maintain circulation, further elevating systolic pressure. For individuals with hypertension or cardiovascular conditions, this abrupt rise can pose serious risks. Research suggests these effects are most pronounced during the first three minutes of immersion, emphasizing the need for controlled exposure.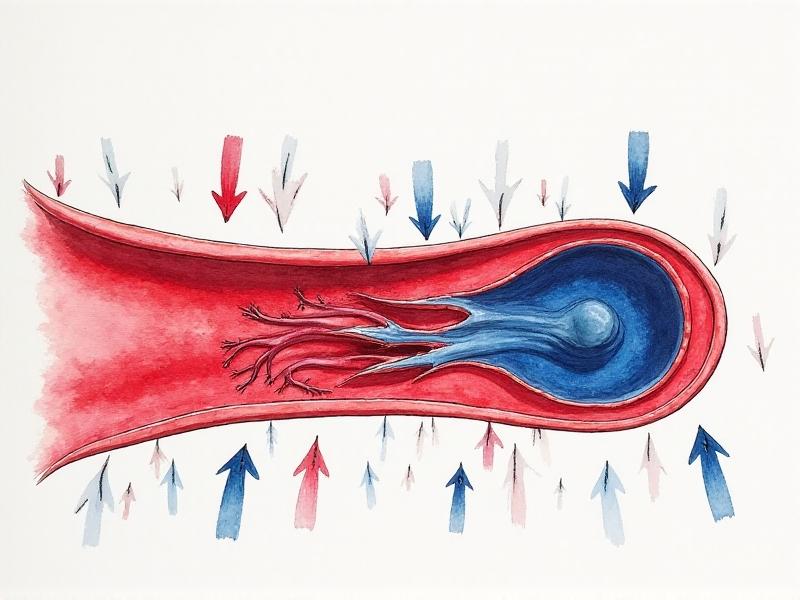
Understanding Blood Pressure Basics: What You’re Measuring
Blood pressure (BP) is the force exerted by circulating blood against artery walls, measured in millimeters of mercury (mmHg). Systolic pressure (the higher number) reflects heart contractions, while diastolic (the lower number) represents relaxation between beats. Normal BP ranges between 90/60 mmHg and 120/80 mmHg. During ice baths, systolic pressure can temporarily rise by 20–30 mmHg. Continuous monitoring helps identify abnormal trends, such as hypertensive crises or arrhythmias, enabling timely intervention. Accurate measurement requires proper cuff placement and stillness—challenging in a shivering, immersed individual.
How Ice Baths Affect Blood Pressure in Real-Time
Studies using continuous BP monitors reveal a biphasic response: an initial surge as the body reacts to cold, followed by a gradual decline as it adapts. However, this stabilization varies widely. Factors like water temperature, immersion depth, and individual health determine the magnitude and duration of BP changes. For example, full submersion up to the neck causes greater cardiovascular strain than partial immersion. Athletes often tolerate these shifts better than untrained individuals, but even healthy users risk dizziness or fainting upon exiting the bath due to rapid vasodilation.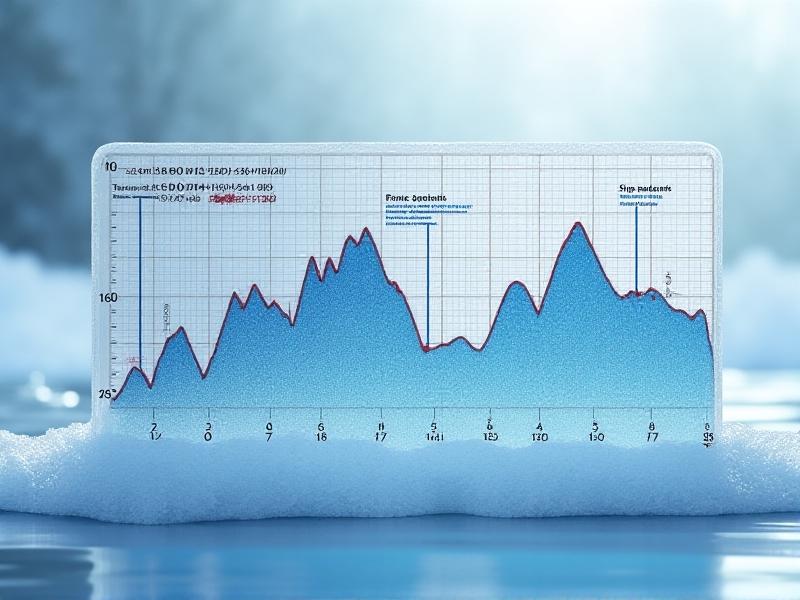
Methods for Monitoring Blood Pressure During Ice Baths
Traditional manual cuffs are impractical during immersion, but wearable technology offers solutions. Wireless devices like chest-strap monitors or finger cuffs can track real-time BP without compromising comfort. However, accuracy may diminish in extreme cold or motion-heavy scenarios. Recent advancements include waterproof smartwatches with optical sensors, though these are better suited for post-immersion analysis. For clinical settings, beat-to-beat monitors using finger arterial pressure waveforms provide precise data but require professional calibration. Regardless of method, baseline measurements before and after baths are essential for context.Risks and Considerations for High-Risk Individuals
Individuals with hypertension, heart disease, or arrhythmias should approach ice baths cautiously. The sudden BP spike can strain weakened arteries, increasing the risk of stroke or cardiac events. Pregnant women, elderly individuals, and those with Raynaud’s disease are also vulnerable. Consultation with a healthcare provider is non-negotiable for these groups. Even for low-risk users, gradual acclimatization—starting with shorter durations and higher temperatures—helps the body adapt safely. Recognizing warning signs like chest pain, numbness, or severe headache is crucial for immediate cessation.Best Practices for Safe Ice Bath Experiences
To minimize risks, limit immersion to 5–10 minutes and avoid submerging beyond the waist initially. Pairing ice baths with controlled breathing techniques (e.g., box breathing) can mitigate stress responses. Post-bath, warm up gradually—avoid hot showers, which can exacerbate BP fluctuations. Hydration and electrolyte balance also play a role; dehydration exacerbates cardiovascular strain. Always monitor BP 10–15 minutes post-immersion to ensure it returns to baseline. Partner supervision adds an extra layer of safety, particularly for beginners.The Future of Cold Therapy and Blood Pressure Research
Emerging studies explore personalized cold therapy protocols based on real-time biometrics. Innovations like AI-driven apps could tailor immersion times and temperatures to individual BP responses. Researchers are also investigating whether repeated cold exposure induces long-term cardiovascular adaptations, akin to high-altitude training. Meanwhile, non-invasive monitoring tools are becoming more accessible, empowering users to make data-informed decisions. As interest grows, bridging the gap between anecdotal benefits and evidence-based guidelines will be key to maximizing safety and efficacy.Advertisement
Recommended Reading: Safe Cold Exposure Durations by Water Temperature





















Comments
Leave a Comment
Your email address will not be published. Required fields are marked *